Teaching Module
ULTRASOUND EVALUATION OF THE LSCS SCAR SITE
INTRODUCTION :
The safety of Vaginal Birth After Caesarean (VBAC) has been shown but there are no reliable methods to predict the risks of uterine rupture in these patients.
Studies have shown that ultrasonography may predict uterine rupture in women with previous cesarean delivery. The risk of uterine rupture in the presence of an LSCS scar is related directly to the degree of thinning of the lower uterine segment (LUS).
Although LUS thickness as measured by sonography at or near term is being used by 16% of obstetricians in Canada to determine which women are good candidates for VBAC, the value of applying sonographic LUS thickness measurement in the management of VBAC remains unclear and there are no clear guidelines in this regard.
Very little has been published on sonographic LUS measurement. Issues such as how to measure (ie. the technique), the period of gestation when to measure, normal values, what constitutes scar thinning etc have not been standardized.
The techniques used for measuring the LUS thickness and identifying defects have not been consistent among different studies.
FORMATION OF THE LOWER UTERINE SEGMENT
On the surface of the non-gravid uterus about midway between the apex and base, is a slight constriction, known as the isthmus, and corresponding to this in the interior is a narrowing of the uterine cavity. The portion above the isthmus is termed the body, and that below, the cervix. The isthmus of the uterus is therefore the constricted part of the uterus between the body and the cervix. The length of the isthmus is about 0.5 cm -1 cm and its cavity enters the internal os.
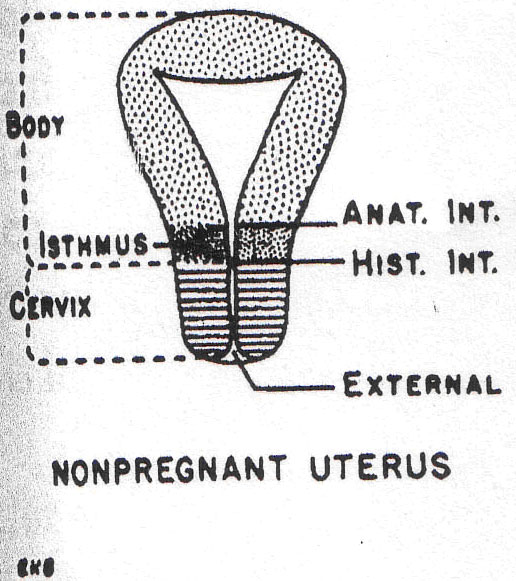
During pregnancy, the isthmus expands from a length of 0.5-1 cm to 2.5 cm at term to become the lower part of the uterine cavity, called the lower uterine segment. Development of the lower uterine segment begins at 28-30weeks gestation. The globular uterus sits on top of the lower uterine segment
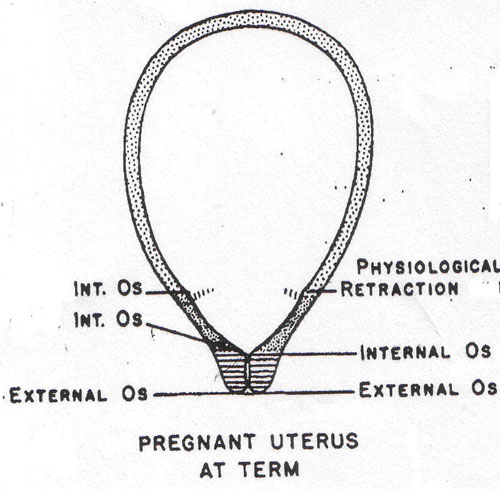
LOCATION OF SCAR OF LSCS :
Scar location is dependent primarily on the degree of cervical effacement DURING the Caesarean operation.
Cesarean section incisions pass through the isthmus if the cervix is not effaced.
Cesarean sections, done during uterine contractions are actually performed through cervical tissue.
WHEN DO WE MEASURE THE SCAR THICKNESS ?
1) Scar thickness is usually measured in the 3rd trimester : Some argue for 36-38 weeks, Some suggest prior to 36 weeks in order to avoid changes in measurement due to head engagement and physiological reduction of liquor
2) Some studies have been done in the 2nd trimester and late 2nd trimester.
3) 1st trimester measurements are also being studied and followed up.
HOW OFTEN CAN WE IDENTIFY THE LSCS SCAR ?
In the third trimester, the scar may not always be identified and instead the thickness of the lower uterine segment is taken. In one study, the previous uterine scar could not be identified in 83% of the cases and instead, a normal-appearing LUS indistinguishable from that in the non-LSCS women was seen.
METHODS/TECHNIQUES OF MEASURING LSCS SCAR THICKNESS :
Patient should not be in labour at the time of scar thickness measurement. The degree of fullness of the urinary bladder affects the thickness of the LUS measurement.
Different methods used to measure thickness of LUS are listed below :
1) TRANS-ABDOMINALLY ON FULL BLADDER :

Measured at 36-38 weeks.
The arrows indicate where the LUS thickness is measured ---- the thinnest zone of the lower segment was identified visually at the midsagittal plane along the cervical canal. This area was magnified and the measurement was taken between the urinary bladder wall�myometrium interface and the myometrium/chorioamniotic membrane� amniotic fluid interface.
2) TRANS-ABDOMINALLY ON EMPTY BLADDER :
Thickness of uterine wall can be measured at the dome of the urinary bladder without including the urinary bladder wall.

3) TRANS-ABDOMINAL ON HALF FULL BLADDER
4) TRANSABDOMINAL INCLUDING THE BLADDER MUCOSA AND THE PERITONEAL LAYER IN THE MEASUREMENT �
This technique was applied by Rozenberg et al who stated that VBAC may be attempted if the LUS thickness is 3.5 mm or more at at 36-38 weeks� gestation
5) TRANS-VAGINAL SONOGRAPHY WITH FULL BLADDER (to the extent that the patient had urge to void):
Measured between 19-39 weeks gestation. The thickness of the urinary bladder was not included in the measurement
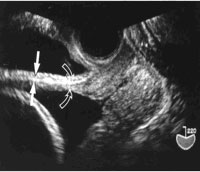
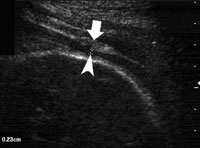
Transvaginal sonography showing the lower uterine segment and bladder full. Open arrow indicates uterine wall; solid arrow indicates bladder wall.
6) MEASUREMENT IN FIRST TRIMESTER :
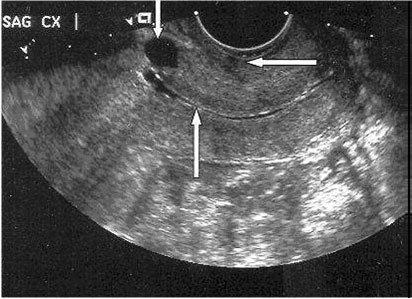
Picture shows measurement of the thickness of lower uterine segment in the 1st trimester using a 7.5 MHz. transvaginal probe.
The cervix and lower uterine segment were visualized in the sagittal plane. The thickness of the anterior wall of the lower uterine segment and the total thickness of the lower uterine segment were measured at the level of the internal os ( placing the calipers at the edge of the internal os and the outer edge of the myometrium).
SHOULD WE MEASURE TRANS-ABDOMINALLY OR TRANS-VAGINALLY ?
Though the last word has yet to be said, in a study Jastrow et al, performed transabdominal and transvaginal sonography, between 36 and 38 weeks of gestation with patients on full and a half-full bladder and concluded that �the agreement between two observers for sonographic transvaginal measurement of the lower uterine segment can be considered good, compared with poor to moderate agreement using the transabdominal approach.�
Also, the degree of fullness of the urinary bladder affects the thickness of the LUS measurement.
However high resolution US scanning trans-abdominally does give very good images and the issue between TVS and TAS measurement has not been concluded.
SCAR THICKNESS � WHAT IS NORMAL and WHAT CAN BE CALLED THINNING?
Thickness of the LUS decreases as gestational age advances.
Prior cesarean delivery is associated with a sonographically thinner LUS when compared with those with prior vaginal delivery. This difference in thickness of the lower uterine segment between those with prior Caesarean delivery and prior vaginal delivery was found to become apparent only after 29 weeks.
Rozenberg et al indicated that the risk of uterine rupture in the presence of a defective scar was related directly to the degree of thinning of the lower uterine segment as measured by transabdominal ultrasonography at or near 37 weeks� gestation. In particular, they demonstrated that this risk increased significantly when the thickness was 3.5 mm or less ( It is necessary to note that their method of measurement was trans-abdominal and included the thickness of the urinary bladder mucosa and the peritoneal layer) . They recommended that VBAC (vaginal birth after Caesarean) may be attempted if the thickness of the LUS was at least 3.5 mm.
Fukuda et al and Suzuki et al, using transabdominal sonography( without clearly defining the site of measurement), concluded that a wall thickness of 2 mm or less was a potential sign of a uterine defect.
Gotoh et al, using transvaginal sonography concluded that 74% of women with a LUS of less than 2.0 mm had an incomplete uterine rupture noted at cesarean delivery.
Michaels et al, instead of just measuring the thickness, described the sonographic appearances of the LUS by its symmetry, thickness, movement, ballooning, and the presence of a wedge defect and divided these findings into 3 classes to assist in identifying uterine defects.
It is obvious that the techniques used for measuring the LUS thickness and identifying uterine defects have not been consistent among different studies.
Also, the cutoff value of the thickness of LUS on sonographic examination which indicates a high risk of uterine rupture has yet to be identified.
Most studies show a high negative predictive value of LUS measurement with respect to the risk of rupture and therefore obstetricians offer patients a trial of labor when the LUS thickness is shown to be normal sonographically.
OTHER DESCRIPTORS OF THE SCAR SITE /LUS :
1) Any balloon effect, as described by Michaels et al,11 consisting of any abnormal bulging of the outer layer associated with fetal movement or changes in amniotic fluid pressure against the urinary bladder base, was noted.
2) echotexture of the scar
3) color Doppler study for scar vascularity
Areas of Increased Echogenicity in the Outer Layer With or Without Myometrial Thinning :
In some patients, the previous scar was identified as an isolated thickened echogenic area in the outer layer, whereas the myometrial layer underneath this area appeared asymmetrically thinned out when compared with the adjacent myometrium.
References
1) J Ultrasound Med. 2004 Jul;23(7):907-11; quiz 913-4. Second-trimester sonographic comparison of the lower uterine segment in pregnant women with and without a previous cesarean delivery. Sambaziotis H, Conway C, Figueroa R, Elimian A, Garry D.
2) Ultrasonographic evaluation of lower uterine segment thickness in patients of previous cesarean section. Sen S, Malik S, Salhan S.
Department of Obstetrics and Gynecology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.3) Identifying VBAC patients at risk of uterine rupture - vaginal birth after previous cesarean - adapted from the Lancet 1996;347:281-4 - Tips from Other Journals
4) 1st trimester scar assessment :Prospective Analysis of Routine Ultrasound Screening of Cesarean Scars, Chandler Mohan, M.D. Carlos Torres, M.D. B. Denise Raynor, M.D. ,Presented at the 40th Annual Clinical Topics in Gynecology and Obstetrics and John D. Thompson Resident Research Day Program, Friday, May 12, 2006
5) Journal of Diagnostic Medical Sonography, Vol. 20, No. 6, 418-421 (2004) DOI: 10.1177/8756479304268938 Prenatal Sonographic Detection of Uterine Dehiscence Diane J. Youngs, BS, RDMS, RVT
6) Myometrial Thickness in Pregnancy: Longitudinal Sonographic Study Shimon Degani, MD, Zvi Leibovitz, MD, Israel Shapiro, MD, Ron Gonen, MD, Gonen Ohel, MD
7) Sonographic Evaluation of the Lower Uterine Segment in Patients With Previous Cesarean Delivery . Y. T. Cheung, MBBS, FRCOG, FRCSC, RDMS, Oana C. Constantinescu, MD, RDMS and Birinder S. Ahluwalia, MBBS, RDMS
8) Obstetrics & Gynecology 2000;95:596-600 Predicting Incomplete Uterine Rupture With Vaginal Sonography During the Late Second Trimester in Women With Prior Cesarean HIDEO GOTOH, MD, HIDEAKI MASUZAKI, MD, ATSUSHI YOSHIDA, MD, SHUICHIRO YOSHIMURA, MD, TSUNETAKE MIYAMURA, MD and TADAYUKI ISHIMARU, MD, PhD .From the Department of Obstetrics and Gynecology, Nagasaki University School of Medicine, Nagasaki, Japan.
9) Inter- and intraobserver variability in sonographic measurement of the lower uterine segment after a previous Cesarean section N. Jastrow *, E. Antonelli, R. Robyr, O. Irion, M. Boulvain.Obstetrics and Gynecology Department, University Hospital of Geneva, Switzerland
